What is Acute Coronary Syndrome:
Note:
- Stable angina doesn’t typically change in frequency and it doesn’t worsen over time.
- Unstable angina is chest pain that occurs at rest or with exertion or stress. The pain worsens in frequency and severity.
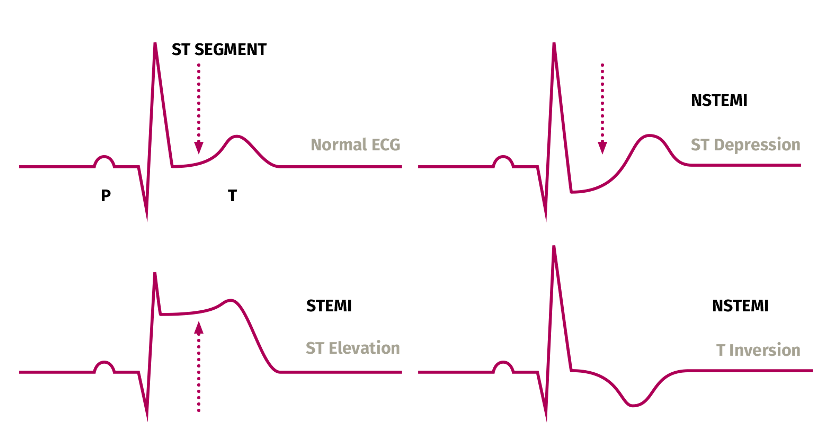
Below is an ECG graph showing the difference in STEMI and NSTEMI
High-sensitivity blood tests for serum troponin are used to differentiate between NSTEMI and unstable angina.
Non Pharmacological Treatment
The decision regarding choice of these management depends on the type of ACS, time since symptom onset, clinical condition of the patient, other co-factors, and their risk of future cardiovascular events
Revascularisation procedures such as percutaneous coronary intervention (PCI)- Primary PCI (if within 12 hours of symptom onset and within 120 minutes of fibrinolysis) is the preferred strategy for most patients.
Coronary artery bypass graft (CABG)
Initial Management
Pain relief should be offered as soon as possible with glyceryl trinitrate (sublingual or buccal). I
Intravenous opioids such as morphine may also be administered, particularly if acute myocardial infarction (MI) is suspected.
A loading dose of aspirin should be given as soon as possible.
All patients admitted to hospital should be closely monitored for hyperglycaemia. Those with a blood-glucose concentration greater than 11.0 mmol/litre should receive insulin—consider administration via a dose-adjusted infusion.
STEMI and NSTEMI Treatment
The management of a STEMI focuses on restoring the coronary blood flow as quickly as possible to reduce mortality.
Aspirin and where appropriate a second antiplatelet agent (prasugrel, ticagrelor, or clopidogrel) should be offered unless aspirin alone may be appropriate for some patients with a high bleeding risk not undergoing a PCI.
Prasugrel is the preferred agent for most patients undergoing a primary PCI (based on benefit vs risk)
For NSTEMI antithrombin therapy with fondaparinux sodium should also be offered, unless the patient is undergoing immediate coronary angiography, or has a high bleeding risk. Alternatively Heparin (unfractionated) may be used in patients with severe renal impairment.
Secondary Prevention of CVD
Lorem ipsum dolor sit amet, at mei dolore tritani repudiandae. In his nemore temporibus consequuntur, vim ad prima vivendum consetetur.